Harnessing the Power of the Immune System: Optimizing T Cell Killing Cancer Immunotherapy
Taken with kind permission from Select Science (Originally published on 29 Oct 2018).
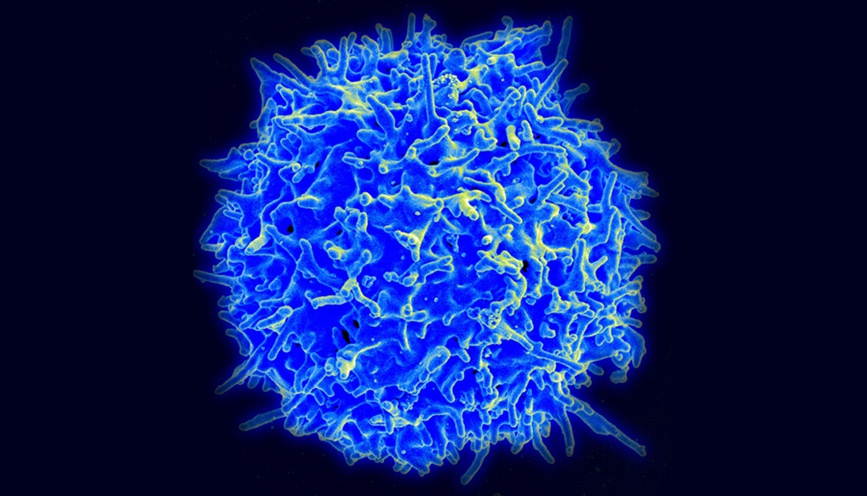
Image: Scanning electron micrograph of a human T cell, courtesy of NIAID (National Institute of Allergy and Infectious Diseases) on Flickr under the Creative Commons license.
Dr Amir Alpert (Senior Scientist Immatics US Inc.) modifies T cell receptors and their targets to seek out better immune therapies for solid tumors
Immunotherapy has emerged as a real game-changer in cancer therapeutics. After decades of research, there is now hope of boosting an individual’s own immune system to fight cancer by tapping into T cell-based therapies. One group of patients particularly benefiting from these new approaches are those with malignancies previously considered ‘difficult to treat’. Novel immune therapies include chimeric antigen receptor T cell (CAR-T) therapy and TCR-based adoptive T cell (TCR-T) therapy.
“My primary focus is to understand how manipulating the T cells outside of the body goes on to increase the therapeutic advantage when we re-infuse them into the body. The final goal is to make a better therapeutic product.” — Dr Amir Alpert
CAR-T therapy versus TCR-T therapy
While CAR-T therapy involves engineering the T cells to express antibody-derived receptors for cancer antigens, TCR-T therapy involves introducing a specific T cell receptor that directs the cell towards tumor cells.
In this SelectScience® interview, we speak with Dr. Amir Alpert, senior scientist at Immatics US Inc., a company lanched by Immatics Biotechnologies GmbH as a Joint Venture with MD Anderson in 2015 to develop multiple TCR-based adoptive T cell therapies targeting cancer.
While CAR-T therapy involves engineering the T cells to express antibody-derived receptors for cancer antigens, TCR-T therapy involves introducing a specific T cell receptor that directs the cells towards tumor cells. Alpert says: “CAR-T therapy is limited in the number of targets it has because it can only search on the surface of the cell. TCR-T therapy, on the other hand, has the advantage that it can address a large number of additional targets due to its ability to recognize intracellular targets as well.”
The killer question
Alpert explains that his current research focus is on cellular therapies for solid tumor malignancies: “We're searching deep into the immune system and across cancer cells to identify the best targets and corresponding T cell receptors. My primary focus is to understand how manipulating the T cells outside of the body goes on to increase the therapeutic advantage when we re-infuse them into the body. The final goal is to make a better therapeutic product.”
One of his lab’s key projects is to identify T cell products able to kill multiple tumor cells compared to those that kill only once or twice and also to understand where this ability comes from – a focus for their research and development team. “We take primary T cells that have been genetically modified with one of our T cell receptors of interest,” says Alpert. “Then we expose them to tumor cell lines that express the antigen specific to that TCR. After one round of exposure and measurement we then re-expose them to additional tumor cells. This is a process that is just reiterated until we no longer see the ability for the T cells to kill the tumor cells.”
Technological solutions
Alpert’s lab uses a variety of techniques — primary cell culture, antiviral transductions, and flow cytometry to phenotype cells — but their workhorse is the IncuCyte S3® live-cell imaging system which gives the team a visual understanding of their in vitro TCR-T assays. One of the main benefits of IncuCyte is in overcoming limitations of previously used end-point assays, where cell cultures were set up, incubated, then harvested at single or possibly multiple time points, thereby requiring a higher number of samples and longer experiment times.
“End-point assays were very tedious and laborious,” Alpert comments. “What the IncuCyte enabled us to do is set up our experiment and allow it to go for a number of hours without being perturbed and then get real-time data tracking of the information. Rather than being restricted to say, a four-hour chromium release assay, we can now do multiple T cell killing assays in a day with the IncuCyte. That was the real advantage. Now we have the ability to extend these assays based on what we're seeing and to make real-time decisions.”
Current limitations, future hopes
In the future, Alpert is planning on creating more complex models ex vivo using the IncuCyte, for example, mixed tumor reactions, mixed lymphocyte reactions, or with T cells plus stimulatory T cells. Hopefully this will help to address what he identifies as one of the current limitations in immunotherapy – finding the right target. “The solid tumor environment is such a difficult landscape to tackle and up-to-date cellular therapy has primarily shown advantages in liquid tumors. I think a big question for immunotherapy will be — will cellular therapy work for solid tumors once we find the right target and the right TCR to use or the right chimeric antigen receptor? We’re going to get a lot of information in the coming years,” he concludes.
